Can we be certain that elevated LDL (Low-density lipoprotein) particles have no meaning and can be completely ignored?
Certainly not.
Can we be certain that all LDL particles are deadly and need to be treated to microscopically low levels?
Certainly not.
So, what do we do?
I have seen countless second opinion consults and enrolled numerous clients in my Boundless Health Program who have this exact question. What’s the deal with LDL? Do we worry or don’t we?
Life is much easier when it is black and white, good and bad. I, however, believe in looking for the nuance and trying to understand things a little deeper.
But first, let’s back up a little.
What is LDL and LDL-P?
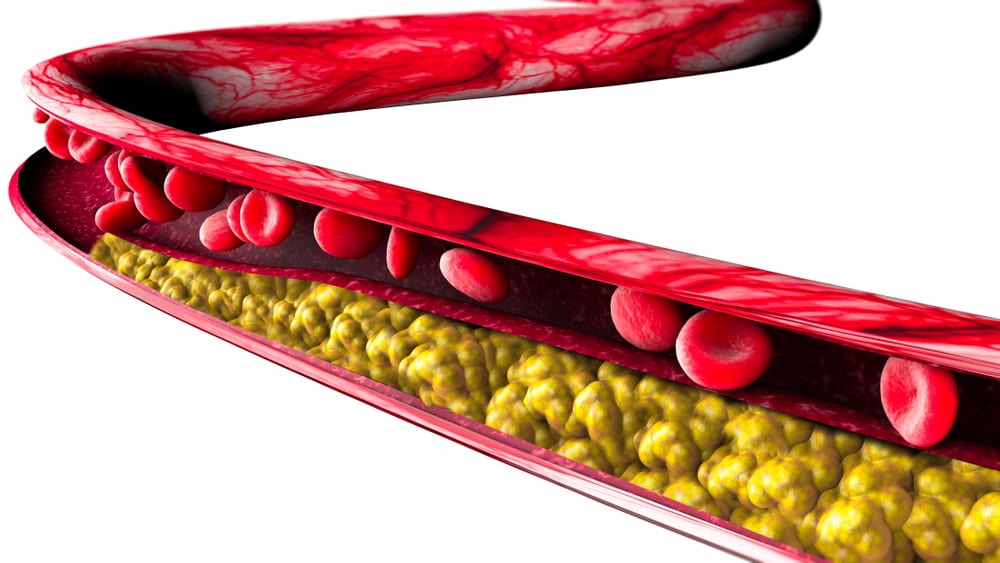
Cholesterol can be a complex topic that we frequently oversimplify, which I am about to do. In brief, LDL is known as the “bad” cholesterol, the cholesterol that is found in plaque buildup in our hearts. But the truth is that LDL is not inherently bad. In fact, LDL has a purpose in our bodies as part of our immune response and as a fuel and vitamin delivery mechanism to name a few. If vascular injury and inflammation are present, then modified LDL may invade vessel walls and participate in a cascade of events leading to plaque buildup and an eventual heart attack.
LDL-C is a measure of the total amount of cholesterol in our LDL lipoproteins. LDL-P is the total number of the LDL lipoproteins. Studies show that LDL-P is a much better marker for CVD risk than LDL-C. As an analogy, the number of cars on the road matter more than the number of people in the cars.
What are the risks of LDL-P?
On the one hand, trials in the general population show that elevated LDL-P is a risk factor for cardiovascular disease (CVD). This includes a combination of observational trials, genetic mutation trials (mendelian randomization), and drug treatment trials.
All things being equal, based on these trials alone, we should want our LDL-P to be low.
But does LDL alone cause heart attacks and death? Or are there other factors involved?
Of course there are other factors involved in CVD. Vascular injury and inflammation being the two most prominent factors.
Can lowering our LDL-P have risks greater than the potential benefits for certain populations?
Absolutely. Since primary prevention statin trials show we have to treat over 200 people for five years to prevent one heart attack with no difference in mortality, it seems reasonable that certain populations will experience more potential risk than reward.
The Low Carb High Fat Reality
How many LDL or statin trials have specifically looked at individuals on a healthy, real foods, LCHF diet?
None. Not a single one.
How many LDL or statin studies have looked specifically at red headed, left handed boys born the second week of March?
None, at least to the best of my knowledge.
This seems glib but bear with me.
Is there any reason to think a red headed, left handed boy born the second week of March would behave any differently than everyone else in these LDL studies? Not really. Especially if they are eating a standard American diet or a low -fat diet as was almost exclusively studied in every cholesterol or statin trial.
Here’s the more important question. Is there reason to believe individuals on a healthy, real foods, LCHF diet would behave any differently than everyone else in the decades of lipid and statin studies?
There absolutely is reason to believe they may behave differently. There is not clear proof, but there is plenty of reason to suspect it.
Think about the benefits of a LCHF lifestyle.
-
Lowers inflammation
-
Reverses insulin resistance
-
Naturally raises HDL and lowers TG
-
Converts majority of LDL particles to larger, more buoyant particles
-
Lowers blood pressure
-
Reduces visceral adiposity
Could these create an environment where an elevated LDL is less of a concern?
It sure could.
To be clear, I openly acknowledge that we do not have definitive proof that we should have no concern with LDL in this situation. In my opinion, this is a specific scenario that the existing trials simply do not address one way or the other.
So, it seems we have two choices.
-
Since we don’t have any proof we can ignore LDL in this setting, we plug the numbers into the 10-year ASCVD calculator and start a statin if the risk is above 7.5%, or we ask the individual to change their lifestyle in hopes the LDL will come down.
-
If the individual is enjoying multiple health benefits from their lifestyle, and they are rightly concerned about the potential risks of statin therapy, then we can follow them for any sign of vascular injury or plaque formation, or any worsening of their inflammatory markers or insulin sensitivity. In the absence of any potentially deleterious changes, we can reason that the risk is low, and the benefits of living the healthy lifestyle may outweigh the risks.
The “problem” is that the second option requires a detailed discussion of the risks and benefits. It requires close monitoring and follow up. It requires us to think outside general guidelines and consider everyone as an individual with their own unique circumstance. These are qualities that our current healthcare system sorely lacks. Yet that is the exact care that each individual deserves.
What do we do in the meantime?
I hope someday soon we will have definitive long-term evidence that a high number of large buoyant LDL particles along with elevated HDL, low TG and low inflammatory markers is perfectly safe.
Until that day, we will have to continue to talk to our patients. To see them as individuals. To weigh the lifestyle benefits with the possible risks. That includes seeing the risks in real numbers- not quoting a 30% benefit with statin therapy. Instead, having a real discussion that statins may reduce your risk a heart attack by 0.6% with an increased risk of muscle aches, an increased risk of diabetes, and a potential increased risk for cognitive and neurological dysfunction.
And we will have to understand that the answer won’t be the same for each person. And we can be OK with that.
So, do you have to worry about your LDL? I don’t know. But I welcome the opportunity to explore the question and reach the best answer for you.
Do you have questions about what your lipids may mean for you? What they mean when taken in the context of your lifestyle and overall health picture? If so, you may want to learn more about my Health Coaching Consult.
Thanks for reading,
Bret Scher, MD FACC