We’re Changing the Cardiology Experience
Because You Deserve Better Care.
The practice of medicine, especially preventive cardiology, is failing patients because it focuses on general guidelines based mostly on numbers: “What’s your LDL?”, “What’s your BMI?” And that’s usually where it stops. It’s dangerous because it focuses on an equation instead of the individual. You are not your numbers. Your body is unique and deserves to be treated as such. We need a transformative shift in cardiology and preventive health care that considers you as an individual.
Let’s Talk
Send us a message and let us know how we can help you.
Introducing
Concierge Preventive Cardiology
with Dr. Scher
What if you could combine…
Now with Dr. Scher’s Concierge Preventative Cardiology, you can!
WELCOME TO
BOUNDLESS HEALTH WITH DR. SCHER
a revolutionary approach to optimizing your health and life!
Find out if this works for you
Connect with Dr. Scher today to see if this model is right for you.
Let’s Talk
Send us a message and let us know how we can help you.
Meet Dr. Scher, MD
CREATOR OF CONCIERGE PREVENTIVE CARDIOLOGY

Hi, I’m Dr. Bret Scher, and I’m changing the direction of preventive cardiology to better you with the care you deserve. I’m also the CEO and Lead Physician at Boundless Health and the Low Carb Cardiologist. I spent the past 15 years as a frustrated cardiologist. My patients weren’t achieving their optimal health, and I didn’t have the time or resources to guide them. That’s why I am revolutionizing my practice of medicine, and why I sought out additional certifications in lipidology, nutrition, personal training, functional medicine, and behavioral change.
It is through this specialized training and working with thousands of patients I recognized how to provide better care. Your health is too important to trust to guidelines designed for the ‘average’ person. You are not average, nor should you want to be!
I also recognize the need for better access and convenience. That’s the heartbeat behind Concierge Preventive Cardiology: open access so together, we can evaluate every facet of who you are and how you can best achieve your goals.
I’m glad you’re here. It tells me you know you deserve better care. I can’t wait to get started finding your path to true health.
Bret Scher, MD FACC
Board Certified Cardiologist and Lipidologist
Yes, People LOVE Dr. Scher’s Approach

We had an incredible turnout for our Webinar, aimed to help you transform your health in 2019. As a result, we decided to create a blog post that includes the full webinar recording, as well as an overview of the learnings for those that were unable to attend.
Webinar Recording
Webinar Overview
Cardiovascular Disease Is the #1 Killer for Men and Women
- 1/3 of all Americans die from Cardiovascular disease
- Around 92 million Americans are living with CVD
- Every 34 seconds someone suffers a heart attack
- Annual health expenditure and lost productivity from CVD ~$330 billion
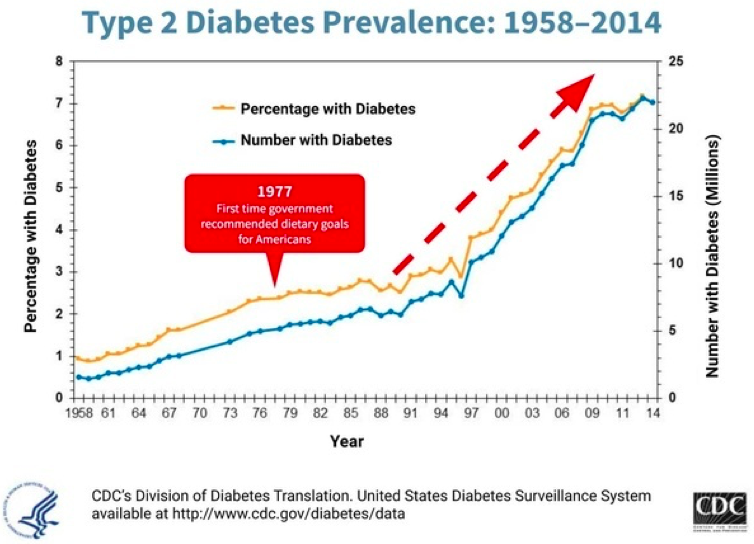
It’s been estimated that 50-80% of these are preventable! Unfortunately, our healthcare system and associated lifestyle guidelines have failed to prevent disease. We could say at best they have failed to prevent heart disease, obesity and diabetes. At worst they have been implicit in its prevalence. While this graph doesn’t show causation, it certainly shows the association of instituting national nutritional guidelines and the rise in diabetes.
Drugs Don’t Fix the Problem
- 60% of Americans take at least 1 prescription drug
- 15% take more than 5 drugs
- Despite this, our overall health and life expectancy continue to decline
HEALTH IS NOT THE ABSENCE OF DISEASE!
In this webinar, we will discuss how to be your own best advocate, why low carb, high fat nutrition should be an option for everyone, and how lifestyle really is the best medicine.
3 Interventions to Improve your Healthcare Experience and Be Your Best Advocate
- Make sure your doc is working with accurate information! Lipids and blood pressure are two prime examples of when doctors make decisions based on limited and faulty information.
- Get your questions answered by writing them down ahead of time so you don’t forget anything and tell your doctor at the beginning of the appointment that you have some questions you’d like to ask at the end.
- Make sure you understand the purpose and benefit of each and every medication. Not some vague answer like “It will improve your cholesterol,” or “It will lower your blood pressure.” Rather, “what impact will it have on my longevity and quality of life?” Will I live longer? Will I feel better? What are the chances the drug will actually benefit me? These are the questions we need answered.
Why Low Carb, High Fat Nutrition Should be an Option for Everyone!
LCHF vs Low Fat Diets
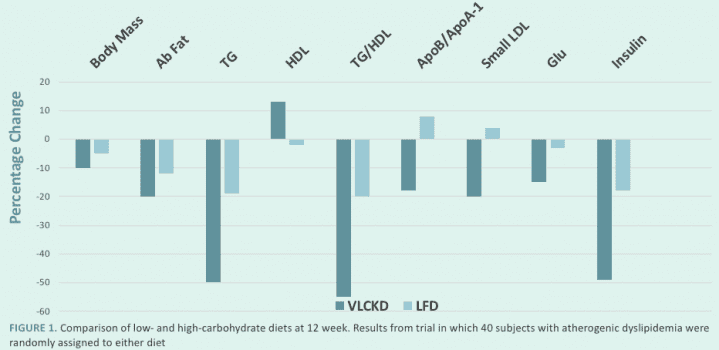
LCHF Benefits
- Decreased hunger, increased energy, mental clarity
- Treats metabolic syndrome/insulin resistance
- Better weight loss
- Improves overall cardiovascular risk for most people
LCHF may not be the best for everyone, but it certainly should be an option for everyone. If you want tips that do work for everyone, follow these bonus tips for weight loss and overall health!
- Don’t drink your calories – even “natural” drinks are full of unnecessary calories. Think about it this way, you would drink a glass of orange juice, but would you really sit down eat the 5 or so oranges it takes to make it? If not, why drink that same amount?
- Get rid of “Food Delivery Systems” – Think about the big sandwiches or burritos we see everywhere in our culture. What is the food? The stuff in the middle! The meat, the cheese, the veggies. What is the unnecessary food delivery system? The bread, the tortilla, the outer layer that has a fraction of the nutrients and a multitude of the carbs!
Lifestyle Really is the Best Medicine!
Science says lifestyle, not drugs, reverse disease:
- NEJM study reported findings on patients at highest genetic risk for heart attack, over 90% more likely to suffer heart attack. Those with healthy lifestyles had a 50% reduced risk with no drugs and no surgeries!
- JACC study found 85% of all heart attacks could be prevented with greater attention to lifestyle.
- A 2018 British Journal of Sports Medicine study found that increasing walking pace to “brisk” for those over 50 reduced all-cause mortality and cardiovascular mortality by 20-24%.
Why is it so hard?
We have all been told that in order to be healthy, we need to eat less, move more, and reduce fat in our diets. But if that is the case, why is it that only 12% of Americans are metabolically healthy, and only 3% of Americans follow a healthy lifestyle?
Because the simple Eat Less, Move More, Reduce Fat approach DOESN’T WORK!!!
I want to assure you that it’s not your fault, you’ve been given the wrong information.
“I was always told I simply didn’t have enough willpower to stick to a diet. I couldn’t understand why I was always hungry and craving foods. I figured it was all genetics. But working with Dr. Scher showed me there is a better lifestyle that I can stick with and still feel great and enjoy my life! Thanks Dr. Scher!”
- E
Keys to Making Lifestyle Change Stick
- Beware of one-size-fits-all nutrition and lifestyle claims
- Individually tailored and flexible nutrition is the key.
- When you eat is just as important as what you eat
- Move your body more
- Get Serious about your sleep
- Don’t be afraid to test and adjust
A Word of Caution
Don’t try to Change Everything at one time.
Choose YOUR most important first step (nutrition, stress, fitness, etc.) and work on that until a new habit is created!
And remember, you don’t have to do it alone! Working with an expert who can help you on your health journey will increase your likelihood for long term success.
As you can see, this was a quick tour to highlight the main points in the webinar. To get the full benefit, I recommend watching the full recording to get all of the context and be able to see the Q&A session at the end.
If you want to get the full experience, here is that recording again:
If you’d like to see the date and content of our next webinar, or be notified when our next webinar will be, please visit our Webinar Page.
I hope you enjoyed this recording, and that we will see you at the next live webinar!
Thanks for reading,
Bret Scher MD FACC
In the fall of 2018, I was diagnosed with Type 2 Diabetes. I was educated enough to know that there was something I could do about it and set out to change the path I was on by adopting a low carbohydrate/Ketogenic Diet to control my blood sugars. Fortunately, it worked right away- but soon after I discovered that I had some red flags on my cholesterol test results. There is a history of Cardiovascular disease in my family and I was disappointed that I might have to yet again make diet changes but was willing to do what was best for my whole health. After an appointment with a local Cardiologist, I felt somewhat confused about how to move forward. I wanted more information and not just a prescription.
I contacted Dr. Scher for a consult because I wanted to confer with someone who not only understood my condition but who could also give me the latest and soundest advice on how I might treat it and move forward in the best way for me as an individual- not as a statistic. I needed someone who came from a low carb perspective as well as a medical background. My interaction with him was positive, informative and went a long way to making me feel like I could make informed choices without the black and white thinking of well-meaning physicians. He sees the WHOLE person and not just one aspect of their health. Wellness is a journey- and having Dr. Scher along the way is a great way to make the trip!
Lisa K.
Can we be certain that elevated LDL (Low-density lipoprotein) particles have no meaning and can be completely ignored?
Certainly not.
Can we be certain that all LDL particles are deadly and need to be treated to microscopically low levels?
Certainly not.
So, what do we do?
I have seen countless second opinion consults and enrolled numerous clients in my Boundless Health Program who have this exact question. What’s the deal with LDL? Do we worry or don’t we?
Life is much easier when it is black and white, good and bad. I, however, believe in looking for the nuance and trying to understand things a little deeper.
But first, let’s back up a little.
What is LDL and LDL-P?
Cholesterol can be a complex topic that we frequently oversimplify, which I am about to do. In brief, LDL is known as the “bad” cholesterol, the cholesterol that is found in plaque buildup in our hearts. But the truth is that LDL is not inherently bad. In fact, LDL has a purpose in our bodies as part of our immune response and as a fuel and vitamin delivery mechanism to name a few. If vascular injury and inflammation are present, then modified LDL may invade vessel walls and participate in a cascade of events leading to plaque buildup and an eventual heart attack.
LDL-C is a measure of the total amount of cholesterol in our LDL lipoproteins. LDL-P is the total number of the LDL lipoproteins. Studies show that LDL-P is a much better marker for CVD risk than LDL-C. As an analogy, the number of cars on the road matter more than the number of people in the cars.
What are the risks of LDL-P?
On the one hand, trials in the general population show that elevated LDL-P is a risk factor for cardiovascular disease (CVD). This includes a combination of observational trials, genetic mutation trials (mendelian randomization), and drug treatment trials.
All things being equal, based on these trials alone, we should want our LDL-P to be low.
But does LDL alone cause heart attacks and death? Or are there other factors involved?
Of course there are other factors involved in CVD. Vascular injury and inflammation being the two most prominent factors.
Can lowering our LDL-P have risks greater than the potential benefits for certain populations?
Absolutely. Since primary prevention statin trials show we have to treat over 200 people for five years to prevent one heart attack with no difference in mortality, it seems reasonable that certain populations will experience more potential risk than reward.
The Low Carb High Fat Reality
How many LDL or statin trials have specifically looked at individuals on a healthy, real foods, LCHF diet?
None. Not a single one.
How many LDL or statin studies have looked specifically at red headed, left handed boys born the second week of March?
None, at least to the best of my knowledge.
This seems glib but bear with me.
Is there any reason to think a red headed, left handed boy born the second week of March would behave any differently than everyone else in these LDL studies? Not really. Especially if they are eating a standard American diet or a low -fat diet as was almost exclusively studied in every cholesterol or statin trial.
Here’s the more important question. Is there reason to believe individuals on a healthy, real foods, LCHF diet would behave any differently than everyone else in the decades of lipid and statin studies?
There absolutely is reason to believe they may behave differently. There is not clear proof, but there is plenty of reason to suspect it.
Think about the benefits of a LCHF lifestyle.
- Lowers inflammation
- Reverses insulin resistance
- Naturally raises HDL and lowers TG
- Converts majority of LDL particles to larger, more buoyant particles
- Lowers blood pressure
- Reduces visceral adiposity
Could these create an environment where an elevated LDL is less of a concern?
It sure could.
To be clear, I openly acknowledge that we do not have definitive proof that we should have no concern with LDL in this situation. In my opinion, this is a specific scenario that the existing trials simply do not address one way or the other.
So, it seems we have two choices.
- Since we don’t have any proof we can ignore LDL in this setting, we plug the numbers into the 10-year ASCVD calculator and start a statin if the risk is above 7.5%, or we ask the individual to change their lifestyle in hopes the LDL will come down.
- If the individual is enjoying multiple health benefits from their lifestyle, and they are rightly concerned about the potential risks of statin therapy, then we can follow them for any sign of vascular injury or plaque formation, or any worsening of their inflammatory markers or insulin sensitivity. In the absence of any potentially deleterious changes, we can reason that the risk is low, and the benefits of living the healthy lifestyle may outweigh the risks.
The “problem” is that the second option requires a detailed discussion of the risks and benefits. It requires close monitoring and follow up. It requires us to think outside general guidelines and consider everyone as an individual with their own unique circumstance. These are qualities that our current healthcare system sorely lacks. Yet that is the exact care that each individual deserves.
What do we do in the meantime?
I hope someday soon we will have definitive long-term evidence that a high number of large buoyant LDL particles along with elevated HDL, low TG and low inflammatory markers is perfectly safe.
Until that day, we will have to continue to talk to our patients. To see them as individuals. To weigh the lifestyle benefits with the possible risks. That includes seeing the risks in real numbers- not quoting a 30% benefit with statin therapy. Instead, having a real discussion that statins may reduce your risk a heart attack by 0.6% with an increased risk of muscle aches, an increased risk of diabetes, and a potential increased risk for cognitive and neurological dysfunction.
And we will have to understand that the answer won’t be the same for each person. And we can be OK with that.
So, do you have to worry about your LDL? I don’t know. But I welcome the opportunity to explore the question and reach the best answer for you.
Do you have questions about what your lipids may mean for you? What they mean when taken in the context of your lifestyle and overall health picture? If so, you may want to learn more about my Health Coaching Consult.
Thanks for reading,
Bret Scher, MD FACC

A new study published in the European Heart Journal says we should care about blood levels of a metabolite trimethylamine N-oxide (TMAO), but is that true?
NBC News: Study explains how red meat raises heart disease risk
For starters, this was a well run and controlled study. Researchers randomly assigned 133 subjects to one of three isocaloric diets with the only difference being the presence of red meat, white meat, or vegetarian protein. Similar to the study by Dr. Ludwig that we referenced earlier, a strength of this study was that the study team supplied all meals for the subjects. Therefore, there was no guessing about what the subjects ate or if they complied with the recommendations. That makes this a strong nutritional study.
Subjects stayed on each diet for four weeks and then had a washout period before transitioning to the next diet. The main take home is that eating red meat increases the blood level of TMAO, which declines after four weeks off the red meat diet. As described in the article:
a red meat diet raises systemic TMAO levels by three different mechanisms: (i) enhanced nutrient density of dietary TMA precursors; (ii) increased microbial TMA/TMAO production from carnitine, but not choline; and (iii) reduced renal TMAO excretion. Interestingly, discontinuation of dietary red meat reduced plasma TMAO within 4 weeks.
It is important to note in our era of frequent conflicts of interest, NBC news reported that the lead investigator for the study is “working on a drug that would lower TMAO levels.” While that in no way invalidates the findings, it does legitimately raise suspicion for their importance.
Interestingly, the study did not test eggs, another food reportedly linked to TMAO. They did, however, note that increased choline intake, the proposed “culprit” in eggs, had no impact on TMAO levels.
The study also did not investigate fish. Fish, traditionally promoted as “heart healthy,” has substantially higher concentrations of TMAO than meat or eggs. One thought, therefore, is that high TMAO levels are produced by gut bacteria rather than the food itself. Although this is an unproven hypothesis, it would also explain variability among subjects.
Now for the harder question. Does any of this data matter? For this study to be noteworthy, we have to accept the assumption that TMAO is a reliable and causative marker of heart disease.
The main NEJM study linking TMAO to an increased risk of cardiovascular disease is not as conclusive as many promote. First of all, only those at the upper quartile of TMAO level had a significant increase in cardiovascular disease risk. Lower elevations had no significant correlation.
Second, those with increased TMAO and cardiovascular disease risk also were more likely to have diabetes, hypertension and a prior heart attack; furthermore, they were older, and their inflammation markers, including myeloperoxidase, a measurement of LDL inflammation, were significantly higher. With so many confounding variables, it is impossible to say the TMAO had anything to do with the increased cardiovascular disease risk.
This study in JACC that saw a correlation with TMAO and complexity of coronary lesions, also found an increased incidence of diabetes, hypertension, older age in the high TMAO group.
Finally, this study found no association at all between TMAO levels and increased risk of cardiovascular disease.
Based on these mixed findings, the jury is still out, and we have plenty of reason to question the importance of elevated TMAO as an independent risk marker or causative factor of coronary disease.
Most importantly, however, since multiple studies continue to show no significant association between meat and egg consumption and increased heart attacks or mortality risk (references here, here, here, here and here) the weak surrogate markers don’t seem likely to matter much. Don’t get caught in the minutiae. Focus on a real-food diet that helps you feel better and improves the vast majority of your markers. And if you have elevated TMAO, the studies suggest you should also check your blood pressure, blood sugars, and inflammatory markers as they may also be elevated. In my opinion, until we have much more convincing data on TMAO, you are far better off targeting those more basic parameters than a blood test of questionable value.
Thanks for reading,
Bret Scher, MD FACC

There’s a common assumption in the medical and nutrition world that a low carb, high fat diet, like a ketogenic diet, will automatically increase one’s risk for heart disease. However, it’s crucial for us to realize that this assumption is inaccurate and not supported by data.
In fact, it’s been well documented that low carb diets can help someone reverse type 2 diabetes and improve metabolic health, changes that dramatically lower one’s cardiac risk. Research and clinical experience supports that a properly formulated low-carb diet can help someone improve, rather than worsen, their heart health.
But many may wonder, how can this be true when I’ve heard that eating fat is bad for us and bad for our hearts?
A big problem comes from assuming that our bodies react the same way to a diet high in carbs + fat as we do to a diet LOW in carbs and high in fat. The truth is that our bodies react dramatically differently to those two versions of a high-fat diet.
How It Works
You see, when we eat lots of carbs, our body uses the carbs as fuel first. Therefore, we won’t burn the fat for energy, and we end up storing it as adipose or fat stores. But when we eat a very low carb diet, our bodies prefer to burn the fat for energy, and therefore there is much less left over to store as body fat. This is dramatically different from a high carb diet!
Studies also demonstrate that people eating a low carb, high fat diet naturally reduce their calories, thus eating less and losing weight seemingly without trying. But those eating high fat and high carb diets tend to eat more calories and gain weight.
So you can see how we can’t just refer to a “high fat diet” as if it is one thing. It makes a big difference if it is also a high carb or low carb diet.
The Main Contributors
Let’s review the main contributors to heart disease, and see how a low carb, high fat diet impacts them.
1- Blood pressure
One study demonstrated a ketogenic diet lowers blood pressure better than the DASH diet, the diet previously felt to be the best for blood pressure management. And others have shown safe and effective blood pressure lowering when starting a low carb, high fat diet that is similar to a low-fat diet.
2- Type 2 Diabetes
Numerous studies demonstrate the efficacy of low carb diets for treating and even reversing type 2 diabetes. Since diabetes is a major contributor to heart disease, reversing it will significantly improve one’s heart health.
3- Inflammation
Ketogenic diets have been shown to reduce many markers of inflammation, including the commonly used CRP.
4- Triglycerides and HDL cholesterol
Having low triglycerides and normal to mildly elevated HDL cholesterol levels are predictive markers of better heart health, likely because they occur with good metabolic health. Numerous studies demonstrate that ketogenic diets reliably help lower triglycerides and raise HDL, thus improving overall cardiac risk.
5- LDL cholesterol
Many assume that high fat diets raise LDL cholesterol. But again, that is not the case. Multiple studies demonstrate no net change in LDL on a ketogenic diet compared to a low fat diet. In fact, one analysis of multiple studies found a net reduction in LDL particles for those following a ketogenic diet.
Important to Note
However, there is a subset of individuals who can see a dramatic rise in their LDL cholesterol when following a ketogenic diet. These so-called Lean Mass Hyper Responders, have unique physiology that predisposes them to an increase in LDL. But it’s important to realize that these individuals are the minority, not the majority. And there’s even emerging evidence suggesting that elevated LDL may not place these individuals at a higher risk, although with much still to learn.
In Summary
The data does not support the assumption that low carb, high fat diets increase heart disease risk. In fact, many studies demonstrate overall improvement in most, if not all, cardiac risk factors. We need to stop assuming all high fat diets are the same, and realize the unique heart health-improving impact of low carb/high fat diets.
If you would like to learn more about the misperception and misunderstanding about ketosis and heart disease risk, please see the video links listed here:
Does Keto Cause Heart Disease?
Debunking a study claiming low carb diets cause heart disease
Analysis of a study demonstrating lowering of cardiac risk with low
carb diets
Thanks for reading,
Bret Scher MD FACC
TAKING YOUR NEXT STEP
WITH BOUNDLESS HEALTH AND DR. SCHER
We are excited to help you in your quest for better health! If you are ready to take the next step, your annual membership will give you access to:
START A CONVERSATION
Connect with Dr. Scher to see if this model is right for you today.
Let’s Talk
Send us a message and let us know how we can help you.
