We’re Changing the Cardiology Experience
Because You Deserve Better Care.
The practice of medicine, especially preventive cardiology, is failing patients because it focuses on general guidelines based mostly on numbers: “What’s your LDL?”, “What’s your BMI?” And that’s usually where it stops. It’s dangerous because it focuses on an equation instead of the individual. You are not your numbers. Your body is unique and deserves to be treated as such. We need a transformative shift in cardiology and preventive health care that considers you as an individual.
Let’s Talk
Send us a message and let us know how we can help you.
Introducing
Concierge Preventive Cardiology
with Dr. Scher
What if you could combine…
Now with Dr. Scher’s Concierge Preventative Cardiology, you can!
WELCOME TO
BOUNDLESS HEALTH WITH DR. SCHER
a revolutionary approach to optimizing your health and life!
Find out if this works for you
Connect with Dr. Scher today to see if this model is right for you.
Let’s Talk
Send us a message and let us know how we can help you.
Meet Dr. Scher, MD
CREATOR OF CONCIERGE PREVENTIVE CARDIOLOGY

Hi, I’m Dr. Bret Scher, and I’m changing the direction of preventive cardiology to better you with the care you deserve. I’m also the CEO and Lead Physician at Boundless Health and the Low Carb Cardiologist. I spent the past 15 years as a frustrated cardiologist. My patients weren’t achieving their optimal health, and I didn’t have the time or resources to guide them. That’s why I am revolutionizing my practice of medicine, and why I sought out additional certifications in lipidology, nutrition, personal training, functional medicine, and behavioral change.
It is through this specialized training and working with thousands of patients I recognized how to provide better care. Your health is too important to trust to guidelines designed for the ‘average’ person. You are not average, nor should you want to be!
I also recognize the need for better access and convenience. That’s the heartbeat behind Concierge Preventive Cardiology: open access so together, we can evaluate every facet of who you are and how you can best achieve your goals.
I’m glad you’re here. It tells me you know you deserve better care. I can’t wait to get started finding your path to true health.
Bret Scher, MD FACC
Board Certified Cardiologist and Lipidologist
Yes, People LOVE Dr. Scher’s Approach

Did you know changing the way you eat may be able to normalize your blood pressure completely? For many people it’s true. But what’s surprising is that it isn’t changing to the diet that most doctors and dieticians recommend.
The DASH diet, Dietary Approach to Stop Hypertension, has long been the “go-to” diet for reducing blood pressure. The DASH diet is a high carbohydrate, low fat diet that recommendseating plenty of fruits, veggies, whole grains, and limiting salt and saturated fat. And while that works for some people, many others can normalize their blood pressure with a nearly opposite approach.
A 2023 study published in The Annals of Family Medicine, demonstrated that a very low carbohydrate diet with no limitations on the amount of salt or the amount or type of fat eaten was better at lowering blood pressure compared to the DASH diet.
Many wonder how this could be, but the answer is pretty straightforward.
Poor metabolic health, from insulin resistance to type 2 diabetes, is a leading cause of high blood pressure. And low carb diets are one of the best lifestyle approaches for improving or even normalizing metabolic health. Therefore, it makes complete sense that a low carb diet would be highly effective at normalizing blood pressure.
Of course there are many other ways to improve blood pressure, such as quitting drugs, tobacco and alcohol, getting regular exercise, managing stress, etc. And these are very important. But since everyone has to eat, it is powerful to eat in a way that can normalize blood pressure.
Let’s explore four ways how low carb diets can help blood pressure.
1- Weight loss
Having overweight or obesity is a strong contributing factor to high blood pressure. And while low-carb eating isn’t the only way to lose weight, it tends to be as good as or even better than low fat eating for weight loss. Some publications even demonstrate weight loss on par with highly effective GLP1 weight loss drugs like Ozemipic and Wegovy.
2- improved metabolic health
As mentioned, metabolic dysfunction is a clear trigger for elevated blood pressure. And while low carb eating isn’t the only way to improve metabolic health, it is likely the most effective dietary pattern for improving metabolic health, and can even do so with or without weight loss.
3- Ketosis
If someone lowers their carbohydrate intake enough, they can enter a state of ketosis, a normal physiologic state where we burn primarily fat for energy instead of carbohydrates. When this occurs, our insulin levels drop to a normal level and we have a natural diuresis, meaning we eliminate sodium and water more than usual. This can help lower blood pressure above and beyond weight loss.
4- Avoiding processed foods
Most well formulated low carb diets avoid highly processed junk foods like potato chips, candy, doughnuts, etc. that can lead to high blood pressure. So, simply eliminating these foods can also contribute to lower blood pressure.
What about salt?
One of the big misconceptions about blood pressure is that we all need to lower our salt intake for better blood pressure. However, this appears to be a gross over-generalization. There’s a growing understanding that a minority of individuals have “salt sensitive” hypertension. This means that the majority are unlikely to affect their blood pressure by altering their salt intake.
Furthermore, where we get our salt likely makes a difference. For insurance, if someone is getting their salt from highly processed foods like chips, pretzels, etc, they are hit with an ultra-processed combination of salt, calories, carbs, and sugars that is bound to raise blood pressure.
But what if someone is eating whole foods like broccoli, cauliflower, steak, and avocado, and they add salt to that meal? Clinical experience suggests our bodies react much differently to this type of salt exposure, and people can dramatically lower their blood pressure despite adding salt to their diet.
Low Carb Eating Works
So while it may not be the right approach for everyone, it is increasingly clear that eating a well-formulated low carb diet is a safe and effective way to lower blood pressure. It’s time to include low carb diets as a first line treatment option for normalizing blood pressure.
Thanks for reading!
Bret Scher MD FACC

Is the Keto Diet Heart Healthy? 7 Reasons Why This Cardiologist Agrees
I am a board certified, card-carrying cardiologist, and I want my clients to eat more fat, more meat, more cheese, more eggs, more avocado, more, more, more.
For decades medical establishments have convinced us to eat low fat, higher carb diets. How has that worked for our health? Here’s a hint, we have record numbers of obesity, diabetes and dementia. Yet, as a cardiologist, that’s the party line I am supposed to support.
But I can’t. It’s just wrong, and I can’t support that line of thinking, not for a second.
Instead, I am a Low Carb Cardiologist. Here are the top Seven reasons why
- Reducing Insulin is Essential to Health and Weight Loss.
Insulin is a hormone naturally secreted by the pancreas to help regulate blood sugar levels. Everything we eat (except possibly for 100% fat meals) causes insulin to rise. That is normal physiology. The problem occurs when our bodies become resistant to the effects of insulin, thus requiring our pancreas to make more and more and more insulin.The problem? Insulin promotes fat storage, increase inflammation and oxidation, and can even help fuel the growth of cancer cells. Therefore, the healthiest approach is one which reduced the level of insulin to the lowest possible levels. As it happens, a Low-carb High-fat or ketogenic lifestyle (LCHF/Keto lifestyle) dramatically improves your body’s sensitivity to insulin, reduces the amount of insulin secreted, and it allows your body to naturally use your fat stores for what they are designed for: Break them down into energy! Once we see that we need to fight chronic elevations of insulin, it becomes obvious why a low-fat diet is harmful, and why a low carb diet is the true path to health. - Eating Fat Improves Your Cholesterol!
Wait, what? Eating fat can improve my cholesterol? Sounds crazy, right? That goes against everything we have heard from the medical establishment. Notice I said “cholesterol.” I didn’t say the “bad” low density lipoprotein (LDL), I didn’t say the “good” high density lipoprotein (HDL), or any one specific type of cholesterol. We have over emphasized the solitary variable of LDL for too long. Total cholesterol to HDL ratio, Triglyceride to HDL ratio, lipoprotein size and density, insulin sensitivity, and other metabolic measures are more powerful predictors of cardiovascular health than just LDL.Once again, we see that all these markers improve with a Low Carb High Fat (LCHF) lifestyle. The medical establishment needs to realize that we are more complicated than one lab value. The key is to look at the whole picture, and this picture dramatically improves with a LCHF lifestyle.If you want to learn more about lipids and cholesterol, I recommend checking out my new dedicated cholesterol course: The Truth About Lipids. - Higher HDL is Associated with a Lower Risk of Heart Disease.
HDL is your friend, but drugs are not. Observational evidence has consistently shown that higher HDL is associated with a lower risk of cardiovascular disease. However, our healthcare establishment does not prioritize HDL for one simple reason- Drugs that raise HDL don’t make you healthier. Trial after trial has failed to show any benefit from drugs that significantly increase HDL.Instead, it’s the HDL-raising lifestyle that provides the benefit, not artificially increasing it with drugs. What’s the best lifestyle to naturally raise HDL? You guessed it. LCHF/Keto lifestyle. Add in some resistance training and you have your friendly HDL climbing the way it was meant to…Naturally. - LCHF Leaves You Feeling Great, Leading to Healthier Decisions
What kind of health decisions do you make when you are fatigued, achy, and find it difficult to concentrate? That’s a rhetorical question, I already know the answer. When things look glum and we don’t feel well, it’s far too easy to sit on the couch or reach for the chips and cookies. Compare those decisions to those you make when you are well rested, energetic, and seeing the world more clearly. For most people, the better you feel, the better decisions you make.Guess what? The majority of people who change to a LCHF lifestyle feel better! It may take a few days or weeks, but in general, they feel more in control of their health, more energetic, and they are able to make better health decisions. I admit this is difficult to prove in a scientific trial. That is why we all should become our own n=1 scientific trial. How do you feel and how are your health decisions after going to a LCHF lifestyle? What matters most is what works for you, not what works for hundreds of people who are kinda-sorta like you. - Keto helps you with fasting.
Eating better helps you not eat. People who eat a high carb diet eat a lot, don’t they? They are always grazing and snacking. Our bodies go through the roller coaster of blood sugar and insulin spikes, making it a challenge to go 24, 18, or even 6 hours without eating. This creates a constant, unwavering supply of insulin in our blood stream.Why is this harmful? For one, it promotes fat storage and keeps us from using our fat as fuel. Secondly, chronically elevated insulin can predispose to heart disease, strokes, cancer, dementia and other devastating health conditions. When people change to Keto, however, they realize they do not need to eat nearly as much or as frequently. Avoiding the carbs and increasing the fats keeps us full longer, and our bodies quickly adapt to longer periods without eating. The result? We can use our fat stores for what they were designed- a source of fuel! It also allows our body to maintain lower insulin levels, and also allows our cells to take care of their health chores, referred to as Autophagy.If you’re interested in Fasting and want to make sure you’re doing it correctly, download my free Full Guide to Fasting. - LCHF Promotes Health Through Increased Autophagy.
Autopha-What? In medicine we like using fancy words to make us look smart. Autophagy is a big word to describe cellular housekeeping. When we have low enough intake of carbs and protein, or when we do intermittent fasts, our bodies can take care of their “to do” lists. That list includes breaking down weak or damaged cells, recycling the good parts and discarding the rest, and slowing down the processes that can lead to abnormal cell growth (i.e. excess proteins in Alzheimer’s disease, abnormal cancer cells etc.).Admittedly, long term outcome studies evaluating fasting or LCHF and cancer or dementia risk have not been done. But, on the flip side, drug trials to prevent the same are showing no benefit despite hundreds of millions of dollars invested. If you asked me (which you sort of did since you are reading my article), I’d vote for autophagy as a preventative strategy any day. It makes good physiologic sense, and it is so easy to achieve. - With Keto You Will Enjoy Eating Again!
That’s right. A way of eating that helps you lose weight, helps you feel better, improves your health and is actually enjoyable! No fake processed soy products, no cardboard tasting rice cakes. True, it also means no more candy, processed snack foods, doughnuts and danishes. But once you swear them off for a few weeks, and you are eating all the eggs, avocados, nuts, fish, steak, cheese etc. that you want, you won’t miss those old crutches any more. Let the enjoyment begin!
I could go on, but since it seems people like “7 Reason” articles, I will leave it at that.
Now you know the secret: Look at the whole picture. Look for a lifestyle, (not a diet) that helps you feel better, increases your enjoyment, and still benefits your overall health.
Is LCHF/Keto the right lifestyle for you? It just may be. To learn more about Low Carb and Keto, download this free E-Book:
Thanks for reading,
Bret Scher, MD FACC
Founder, Boundless Health
www.LowCarbCardiologist.com
ADDENDUM!!
Since I have published this article, there has been a windfall of media buzz around low carb diets increasing our risk of heart disease or diabetes. Let’s look at where that information came from.
1- A study force feeding mice excessive amounts of industrial omega 6 oils. You can guess what I have to say about that. The article was incredibly helpful, and I immediately stopped force feeding my pet mice industrial seed oils. Thanks goodness for that article. As for how it applies to humans eating real food that contain fat, there is zero correlation.
2- Epidemiological study suggesting those who ate low carb (40% calories from carbs, which by the way is NOT low carb) as measured by two food journals over 25 years had a higher risk of dying. Oh and by the way, at baseline they were heavier, more sedentary, smoked more, and ate fewer veggies. Yet somehow they concluded it must be the low carb diet that “caused” the harm. Once again, it may not be bad science, but it sure was awful interpretation of the science.
In light of those two studies and the hoopla surrounding them, has anything happened to change my mind about a LCHF/keto diet being beneficial for our overall health and our heart health?
Absolutely not.
We still need to individualize our care and our lifestyle for who we are and how our bodies respond. That is always the case regardless of our nutrition, our medications, our exercise etc. As long as we do that, then this cardiologist still believes that LCHF IS HEART HEALTHY!
If you liked this post, you’ll love my free E-Book on Low Carb/Keto Starter tips to help you get started on your LCHF path!
Thanks for reading.

We hear the words Heart Healthy a lot, especially when it comes to our nutrition.
By now, you’re likely used to seeing cereals with the “heart healthy” moniker. Is it really heart healthy? We all too frequently refer to foods as “heart healthy”, or we say that our doctor gave our hearts a “healthy” checkup.
It all sounds nice. But what does it mean? How do we define heart health?
How does LDL Cholesterol affect Heart Health?
Unfortunately, most of our current definitions center around LDL cholesterol concentration. While LDL cholesterol plays a role in heart health, it by no means defines heart health in totality.
In fact, in many cases it is the least important factor.
Our healthcare system has simplified things too much, so as a result we focus on one bad guy, one demon to fight. In reality heart disease is caused, and made more likely to occur, by a constellation of contributing issues.
Elevated blood sugar, elevated insulin levels, inflammation, high blood pressure, poor nutrition, and yes, lipids all contribute to heart health. It does us all an injustice to over simplify it to one single cause.
What food is heart healthy?
Our superficial definition of cardiac risk is how industrial seed oils containing polyunsaturated fatty acids (PUFAs) became known as “heart healthy.”
Studies show that they can lower LDL. But they can also increase inflammation and have no clinical benefit and even increase risk of dying. According to our simplified definitions, that doesn’t stop them from being defined as “heart healthy.”
That’s right! Something that increases our risk of dying is still termed “heart healthy.” How’s that for a backwards medical system?!
Same for blood sugar. If you have a diagnosis of Type 2 Diabetes (DM2) that is a risk for cardiovascular disease. If you don’t have the diagnosis, you are fine. That ignores the disease of insulin resistance that can predate diabetes for decades and increases the risk of heart disease and possibly even cancer and dementia.
Cereal can also be called “heart healthy” as they may minimally lower LDL. But is that a good thing if they contain grains that also worsen your insulin resistance and metabolic syndrome? I say definitely not.
Time has come to stop this basic, simplified evaluation and start looking at the whole picture.
How Low Carb High Fat Diets Improve Heart Health
Low carb high fat diets have been vilified as they can increase LDL. But the fact of the matter is that it does so only in a minority of people. The truth is that they can improve everything else!
These diets reduce blood pressure, reduce inflammation, improve HDL and triglycerides, and reverse diabetes and metabolic syndrome! Shouldn’t that be the definition of “heart healthy” we seek? Instead of focusing on one isolated marker, shouldn’t we define heart health by looking at the whole patient?
Only by opening our eyes and seeing the whole picture of heart healthy lifestyles can we truly make an impact on our cardiovascular risk and achieve the health we deserve.
Join me in demanding more. Demand better.
Thanks for reading,
Bret Scher, MD FACC

We had an incredible turnout for our Webinar, aimed to help you transform your health in 2019. As a result, we decided to create a blog post that includes the full webinar recording, as well as an overview of the learnings for those that were unable to attend.
Webinar Recording
Webinar Overview
Cardiovascular Disease Is the #1 Killer for Men and Women
- 1/3 of all Americans die from Cardiovascular disease
- Around 92 million Americans are living with CVD
- Every 34 seconds someone suffers a heart attack
- Annual health expenditure and lost productivity from CVD ~$330 billion
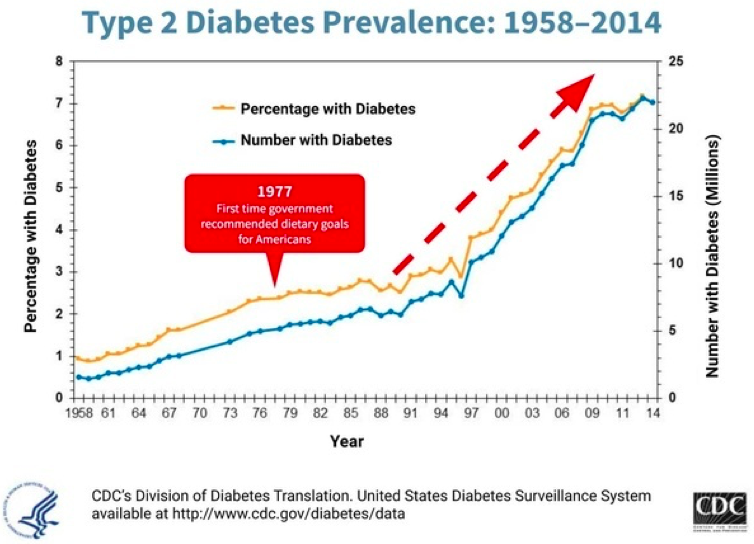
It’s been estimated that 50-80% of these are preventable! Unfortunately, our healthcare system and associated lifestyle guidelines have failed to prevent disease. We could say at best they have failed to prevent heart disease, obesity and diabetes. At worst they have been implicit in its prevalence. While this graph doesn’t show causation, it certainly shows the association of instituting national nutritional guidelines and the rise in diabetes.
Drugs Don’t Fix the Problem
- 60% of Americans take at least 1 prescription drug
- 15% take more than 5 drugs
- Despite this, our overall health and life expectancy continue to decline
HEALTH IS NOT THE ABSENCE OF DISEASE!
In this webinar, we will discuss how to be your own best advocate, why low carb, high fat nutrition should be an option for everyone, and how lifestyle really is the best medicine.
3 Interventions to Improve your Healthcare Experience and Be Your Best Advocate
- Make sure your doc is working with accurate information! Lipids and blood pressure are two prime examples of when doctors make decisions based on limited and faulty information.
- Get your questions answered by writing them down ahead of time so you don’t forget anything and tell your doctor at the beginning of the appointment that you have some questions you’d like to ask at the end.
- Make sure you understand the purpose and benefit of each and every medication. Not some vague answer like “It will improve your cholesterol,” or “It will lower your blood pressure.” Rather, “what impact will it have on my longevity and quality of life?” Will I live longer? Will I feel better? What are the chances the drug will actually benefit me? These are the questions we need answered.
Why Low Carb, High Fat Nutrition Should be an Option for Everyone!
LCHF vs Low Fat Diets
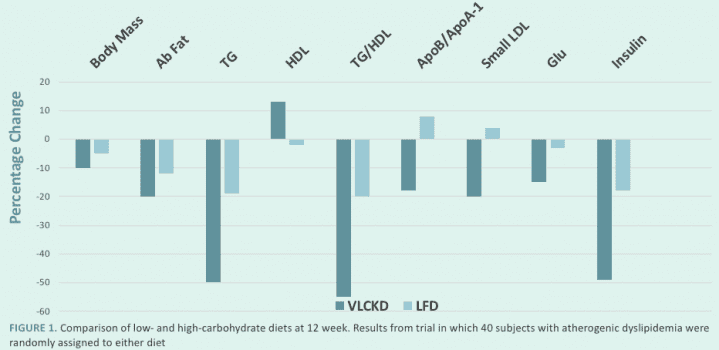
LCHF Benefits
- Decreased hunger, increased energy, mental clarity
- Treats metabolic syndrome/insulin resistance
- Better weight loss
- Improves overall cardiovascular risk for most people
LCHF may not be the best for everyone, but it certainly should be an option for everyone. If you want tips that do work for everyone, follow these bonus tips for weight loss and overall health!
- Don’t drink your calories – even “natural” drinks are full of unnecessary calories. Think about it this way, you would drink a glass of orange juice, but would you really sit down eat the 5 or so oranges it takes to make it? If not, why drink that same amount?
- Get rid of “Food Delivery Systems” – Think about the big sandwiches or burritos we see everywhere in our culture. What is the food? The stuff in the middle! The meat, the cheese, the veggies. What is the unnecessary food delivery system? The bread, the tortilla, the outer layer that has a fraction of the nutrients and a multitude of the carbs!
Lifestyle Really is the Best Medicine!
Science says lifestyle, not drugs, reverse disease:
- NEJM study reported findings on patients at highest genetic risk for heart attack, over 90% more likely to suffer heart attack. Those with healthy lifestyles had a 50% reduced risk with no drugs and no surgeries!
- JACC study found 85% of all heart attacks could be prevented with greater attention to lifestyle.
- A 2018 British Journal of Sports Medicine study found that increasing walking pace to “brisk” for those over 50 reduced all-cause mortality and cardiovascular mortality by 20-24%.
Why is it so hard?
We have all been told that in order to be healthy, we need to eat less, move more, and reduce fat in our diets. But if that is the case, why is it that only 12% of Americans are metabolically healthy, and only 3% of Americans follow a healthy lifestyle?
Because the simple Eat Less, Move More, Reduce Fat approach DOESN’T WORK!!!
I want to assure you that it’s not your fault, you’ve been given the wrong information.
“I was always told I simply didn’t have enough willpower to stick to a diet. I couldn’t understand why I was always hungry and craving foods. I figured it was all genetics. But working with Dr. Scher showed me there is a better lifestyle that I can stick with and still feel great and enjoy my life! Thanks Dr. Scher!”
- E
Keys to Making Lifestyle Change Stick
- Beware of one-size-fits-all nutrition and lifestyle claims
- Individually tailored and flexible nutrition is the key.
- When you eat is just as important as what you eat
- Move your body more
- Get Serious about your sleep
- Don’t be afraid to test and adjust
A Word of Caution
Don’t try to Change Everything at one time.
Choose YOUR most important first step (nutrition, stress, fitness, etc.) and work on that until a new habit is created!
And remember, you don’t have to do it alone! Working with an expert who can help you on your health journey will increase your likelihood for long term success.
As you can see, this was a quick tour to highlight the main points in the webinar. To get the full benefit, I recommend watching the full recording to get all of the context and be able to see the Q&A session at the end.
If you want to get the full experience, here is that recording again:
If you’d like to see the date and content of our next webinar, or be notified when our next webinar will be, please visit our Webinar Page.
I hope you enjoyed this recording, and that we will see you at the next live webinar!
Thanks for reading,
Bret Scher MD FACC

45 million Americans “should” take statins. Are you one of them?
It may surprise you to find out that you might be. When your doctor plugs your information into a cardiac risk calculator, he or she may tell you that you should to take a statin.
You may not feel bad. You may not have many other cardiovascular risk factors. Yet you may be labelled with the “disease” of elevated cholesterol.
“New” Guidelines- Questionable Sources, Questionable Guidelines
Why are so many more previously healthy Americans now being treated for high cholesterol? We can thank the 2013 ACC/AHA guidelines, which increased the intensity with which physicians prescribe statins.
Interestingly, these were not based on any new data. Instead, they were based on new interpretations of old data, much of which has not been made available for third party reviewers. None the less, it is now recommended that physicians consider prescribing a statin to anyone with a 5% 10-year risk of cardiac disease (increased from a previous 20% risk).
To me it seems that a recommendation to dramatically increase the use of these drugs should save lives left and right and have almost no down side. Unfortunately, that is not the case.
Don’t get me wrong. Statins are not useless. They can reduce the incidence of heart attacks and strokes. For someone who has never had a heart attack (referred to as primary prevention) we need to treat between 60 and 104 people for 5 years to prevent one heart attack without any significant difference in the risk of dying.
That’s a little underwhelming, is it not? That seems like a “shotgun” approach where you send a hundred bullets out knowing that one will hit the right person (in this case getting hit by a bullet is a good thing). It doesn’t have to be this way.
In addition, statins are not perfect drugs. For every 50 people treated over five years there will be one new case of diabetes. There will also be at least 10% risk of muscle aches and pains with potential damage to the mitochondria (the energy producing part of the cell), and may even be linked to onset of dementia and memory dysfunction.
A system that potentially harms more people than it helps doesn’t seem like a viable solution to me. We can do better.
Better Define Your Risk
The problem is that our medical culture emphasizes prescribing drugs more than further defining your risk, and more than exploring alternatives to reducing your risk.
The current cardiac risk calculator uses:
- Age
- Gender
- Race
- Total cholesterol
- HDL
- Blood pressure or previous diagnosis of hypertension
- Diagnosis of diabetes
- Smoking status
Those are all reasonable initial risk factors to evaluate. But doesn’t it make sense that if we are using a drug that will only benefit one in 100, maybe we should try to further define those at high risk? To me that is a no-brainer.
For instance, one study showed that by measuring a coronary calcium score on statin eligible individuals, we could reclassify 50% of them so that they no longer “qualify” for statin treatment. We can avoid an enormous number of statin prescriptions with one simple test. A test that is readily available now. A test that has minimal risk (very low radiation dose, and a small chance of incidental findings), and is relatively low cost (about $100).
And we don’t have to stop there.
The Scripps Research Institute has developed an app to allow people to use their genetic information to better define their risks. This could potentially be used to define those who are not at high genetic risk for heart disease and therefore would likely not benefit from statin therapy.
Now we are starting to get somewhere. What if we could better define cardiac risk so that one in 5 people benefit from a statin, as opposed to the current 1 in 100? That is an admirable goal.
Even Better Than A Statin
Once we better define our risk, let’s not forget all the alternative to statins.
One recent study demonstrated that even those at the highest genetic risk for heart disease can cut their risk in half with healthy lifestyle habits (eating healthy, getting regular physical activity, not smoking and not being overweight). And that was the highest risk group! That’s likely just as good as, if not better than, a statin could do.
So why don’t we write prescriptions for intensive healthy lifestyle education programs instead of drugs?
Lifestyle changes are “harder.” Lifestyle changes take longer to see results. Lifestyle changes require more education, encouragement and follow up.
Do you know what else is associated with healthy lifestyle changes? Decreased risk of heart attack, strokes and death. Decreased risk of diabetes, high blood pressure and depression. And the only side effects are feeling better, having more energy, and being in control of your health.
That sounds like something that is well worth the extra work, the needed patience, and the more vigorous follow-up. Don’t you agree?
Start Asking Questions
So, what should you do if your doctor recommends a statin? Start asking questions. Lots of them.
- How high is your calculated cardiovascular risk?
- How much will a statin reduce that risk?
- What else can be done to better define your risk (i.e. coronary calcium score)?
- What else can be done to lower your risk (i.e. intensive lifestyle modifications)?
Ask yourself questions as well.
- How can I improve my nutrition to focus on a vegetable based, real food, Mediterranean style eating that focuses on healthy fats and appropriate proportions of high quality animal products?
- How can I improve my daily physical activities in addition to increasing my weekly exercise?
- How can I improve my stress management and sleep habits?
Remember, the benefits of statins are small. Not zero, but small.
Also, remember that statins have not been directly compared to healthy lifestyle habits. We don’t know if they add anything to a comprehensive lifestyle modification program. In fact, I would wager that if you have healthy eating habits, you get regular physical activity, you exercise regularly, and you practice regular stress management, then statins will not reduce your cardiovascular risk at all.
It may seem like a bold prediction, but to me it seems obvious.
Unfortunately we will likely never see a head-to-head study between statins and healthy lifestyle interventions (I discuss the specifics of the study I would like to see in my prior blog post here).
We can do better than a drug
In the end, remember that we can do better than drugs. We can be in control of our health. We can achieve real health that is not dependent on blood tests or medications.
So, don’t blindly accept a prescription for a statin (or any drug for that matter) without further defining your risk, and without further exploring your alternatives. You and your health deserve at least that much.
Thanks for reading.
Bret Scher, MD FACC
Cardiologist, author, founder of Boundless Health
www.DrBretScher.com
Action Item:
If you are on a statin, or any drug for that matter, make sure you ask your doctor why you are on it, exactly what benefit you should expect, and what the potential short- and long-term side effects are. Also, ask what the alternatives are, specifically regarding your lifestyle and healthy habits. If you aren’t getting adequate answers, ask me! info@drbretscher.com. I welcome your emails.
TAKING YOUR NEXT STEP
WITH BOUNDLESS HEALTH AND DR. SCHER
We are excited to help you in your quest for better health! If you are ready to take the next step, your annual membership will give you access to:
START A CONVERSATION
Connect with Dr. Scher to see if this model is right for you today.
Let’s Talk
Send us a message and let us know how we can help you.
